
HepaHealth II: Preventing liver disease with policy measures to tackle alcohol consumption and obesity
Chronic liver disease (CLD) causes 1.8% of all deaths in Europe. Without policies to mitigate harmful alcohol consumption and obesity, that proportion will continue to increase. This major study, commissioned by EASL and supported by an unrestricted education grant from Bristol-Myers Squibb and Gilead, was carried out over the past 3 years and estimates the impact of policy interventions targeting alcohol and obesity on the incidence of CLD and primary liver cancer in France, the Netherlands, and Romania. The project builds on our previous work published in 2018.
Our peer-reviewed microsimulation model was employed to project trends in alcohol consumption and body mass index (BMI) from 2022 to 2030. We modelled the incidence of CLD and liver cancer under three policy scenarios versus an inaction scenario. All policies had an important impact ranging from a 2% to 7% reduction in annual incidence of CLD and liver cancer by 2030. The most effective scenarios are an increased Minimum Unit Pricing (MUP) of €1 on alcohol or introducing a set of complementary public health policies targeting an increased MUP, a sugar sweetened beverage (SSB) tax, and a volumetric tax that target both alcohol consumption and obesity.
View the poster presented at the EASL Congress in Vienna (June 2023)
Estimating the long-term health impacts of changes in alcohol consumption in England during the COVID-19 pandemic
Alcohol consumption patterns in England changed during the COVID-19 pandemic. Between one-fifth and one-third of adults increased their alcohol consumption, with a similar proportion drinking less. There was a 20% increase in alcohol-specific deaths in England in 2020 compared with 2019, and this trend persisted through 2021. Alcohol harm includes disease morbidity and mortality, healthcare costs, and wider social consequences. This study aimed to quantify future health, healthcare and economic impacts of changes in alcohol consumption observed during the COVID-19 pandemic using the well-validated HealthLumen microsimulation model.
Three alcohol consumption scenarios were looked at, and in all three the model projected a significant increase in the incident cases of disease, mortality, and healthcare costs. If consumption does not return to 2019 levels or lower, the modelling shows that England could see an additional 147,892 cases and 9,914 additional premature deaths from nine alcohol-related diseases, costing the NHS £1.2bn.
The report concludes that a comprehensive alcohol strategy is needed to harmonise policies across the UK, with a coherent set of evidence-based policies: increased resources for alcohol treatment and support; price interventions through the new alcohol duty system; the introduction of minimum unit pricing in England; adding public health as an objective of the licensing system for alcohol outlets; and improving alcohol marketing regulation, to reduce the reach and appeal of marketing to those vulnerable.
View NIHR Report
View Data Appendix
View Results Appendix
View Technical Appendix
View Policy Report from the Institute of Alcohol Studies
View editorial in the British Journal of Hospital Medicine
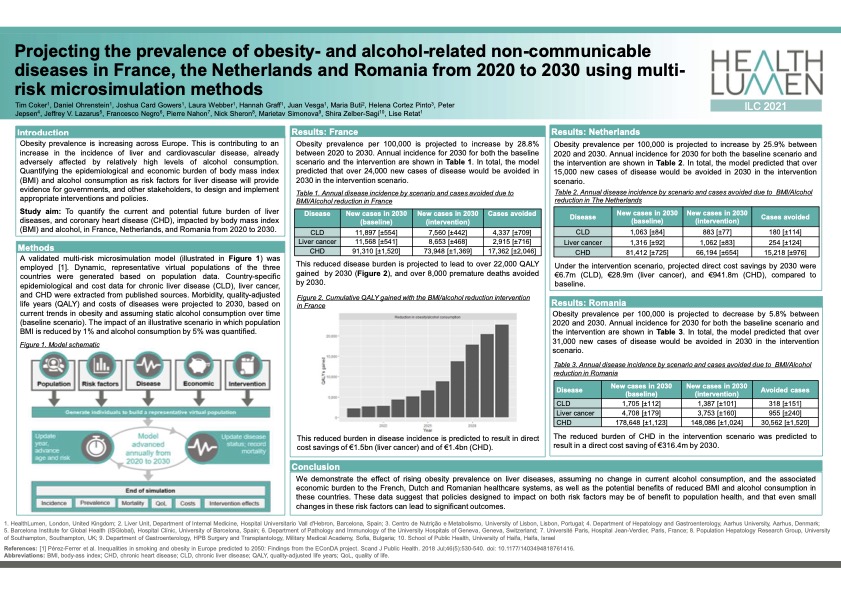
Projecting the prevalence of obesity- and alcohol-related non-communicable diseases in France, the Netherlands and Romania from 2020 to 2030 using multi-risk microsimulation methods
Obesity prevalence is increasing across Europe, which is contributing to an increase in the incidence of liver and cardiovascular disease, already adversely affected by relatively high levels of alcohol consumption. This study demonstrates the effect of rising obesity prevalence on liver diseases, assuming no change in current alcohol consumption, and the associated economic burden to the French, Dutch and Romanian healthcare systems, as well as the potential benefits of reduced BMI and alcohol consumption in these countries. The data suggest that policies designed to impact on both risk factors may be of benefit to population health, and that even small changes in these risk factors can lead to significant outcomes.
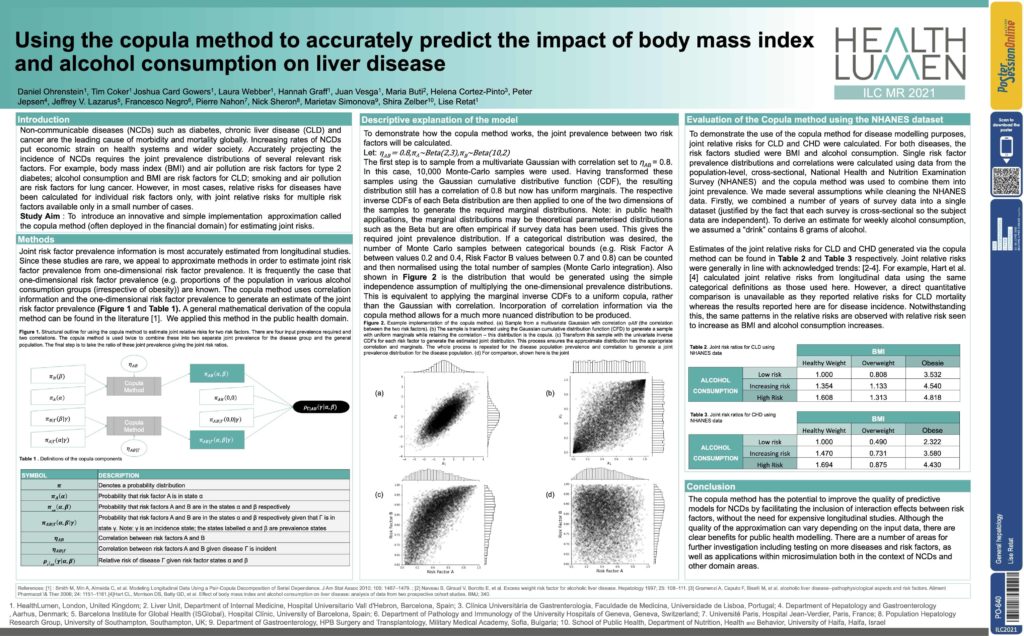
A method for improving NCD modelling using joint risk factors
Accurately projecting the incidence of NCDs requires the joint prevalence distributions of several relevant risk factors. For example, body mass index (BMI) and air pollution are risk factors for type 2 diabetes; alcohol consumption and BMI are risk factors for Chronic Liver Disease; smoking and air pollution are risk factors for lung cancer. However, in most cases, relative risks for diseases have been calculated for individual risk factors only, with joint relative risks for multiple risk factors available only in a small number of cases.
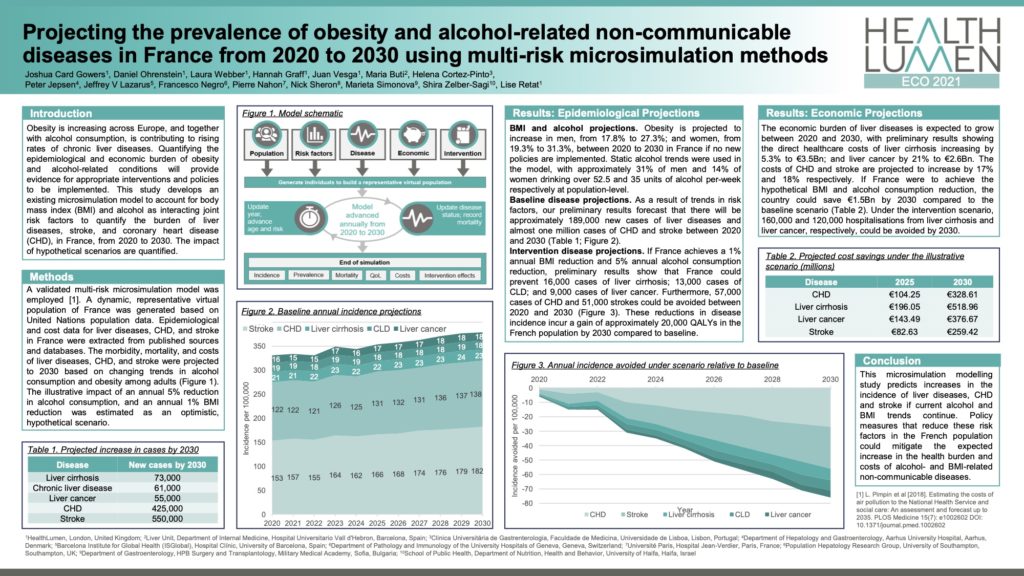
The burden of liver diseases, stroke, and coronary heart disease in France, to 2030
Obesity is increasing across Europe, and together with alcohol consumption, is contributing to rising rates of chronic liver diseases. Quantifying the epidemiological and economic burden of obesity and alcohol-related conditions will provide evidence for appropriate interventions and policies to be implemented. This study develops an existing microsimulation model to account for body mass index(BMI) and alcohol as interacting joint risk factors to quantify the burden of liver diseases, stroke, and coronary heart disease(CHD), in France, from 2020 to 2030. The impact of hypothetical scenarios are quantified.
View overview video