
Inside CKD: Projecting the Population Level Clinical Burden of Chronic Kidney Disease According to Urine Albumin-to-Creatine Ratio (uACR) Categories
This study assessed the future epidemiological and financial burden of CKD using the Inside CKD microsimulation. Specifically, it reports on the CKD population level projections for cardio-renal complications, progression to end stage kidney disease (ESKD), and death due to any cause according to uACR categories.
The results support early intervention in the total CKD population, including individuals with normo- or micro-albuminuria, to reduce cardio-renal outcomes, delay progression to ESKD, and therefore avoid the requirement for costly interventions, including heart related hospitalisations, transplantation and dialysis.
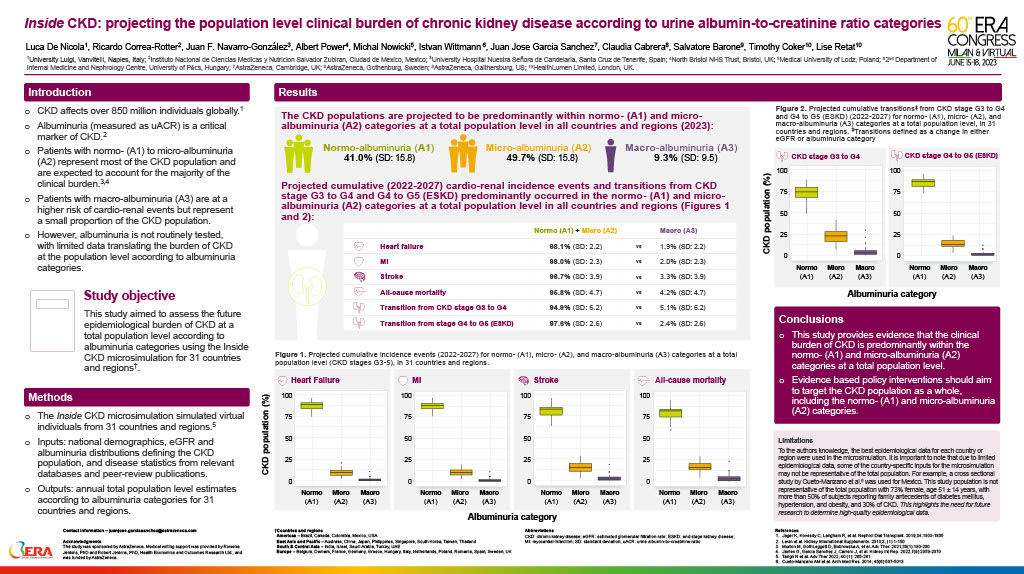
Inside CKD: projecting the population level clinical burden of chronic kidney disease according to urine albumin-to-creatinine ratio categories
This poster, presented at the European Renal Association’s 60th Congress in Milan (June 2023), summarises research on projecting the population level clinical burden of Chronic Kidney Disease (CKD) according to urine albumin-to-creatinine ratio categories. The study provides evidence that the clinical burden of CKD is predominantly within the normo-(A1) and micro-albuminuria (A2) categories at a total population level. Evidence based policy interventions should aim to target the CKD population as a whole, including the normo-(A1) and micro-albuminuria (A2) categories.
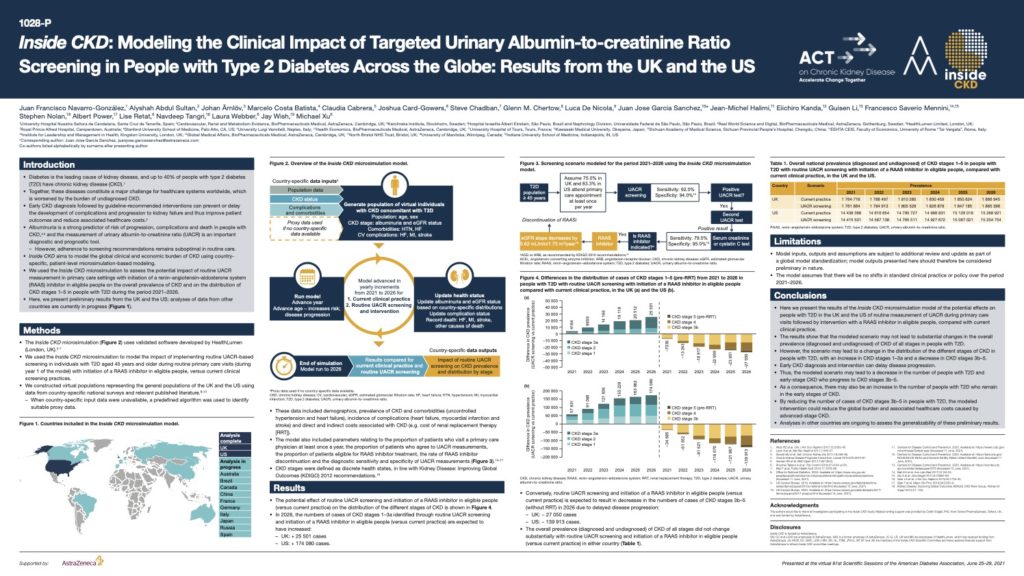
Inside CKD: Modelling the Clinical Impact of Targeted Urinary Albumin-to-creatinine Ratio Screening in People with Type 2 Diabetes Across the Globe
Diabetes is the leading cause of kidney disease, and up to 40% of people with type 2 diabetes (T2D) have chronic kidney disease (CKD) Together, these diseases constitute a major challenge for healthcare systems worldwide, which is worsened by the burden of undiagnosed CKD. Early CKD diagnosis followed by guideline-recommended interventions can prevent or delay the development of complications and progression to kidney failure and thus improve patient outcomes and reduce associated healthcare costs.
Albuminuria is a strong predictor of risk of progression, complications and death in people with CKD and the measurement of urinary albumin-to-creatinine ratio (UACR) is an important diagnostic and prognostic tool.
This poster, presented at the virtual American Diabetes Association’s 81st Scientific Sessions, June 25–29, 2021 demonstrates the potential effects on people with T2D in the UK and the US of routine measurement of UACR during primary care visits followed by intervention with a RAAS inhibitor in eligible people, compared with current clinical practice. By reducing the number of cases of CKD stages 3b–5 in people with T2D, the modelled intervention could reduce the global burden and associated healthcare costs caused by advanced-stage CKD.
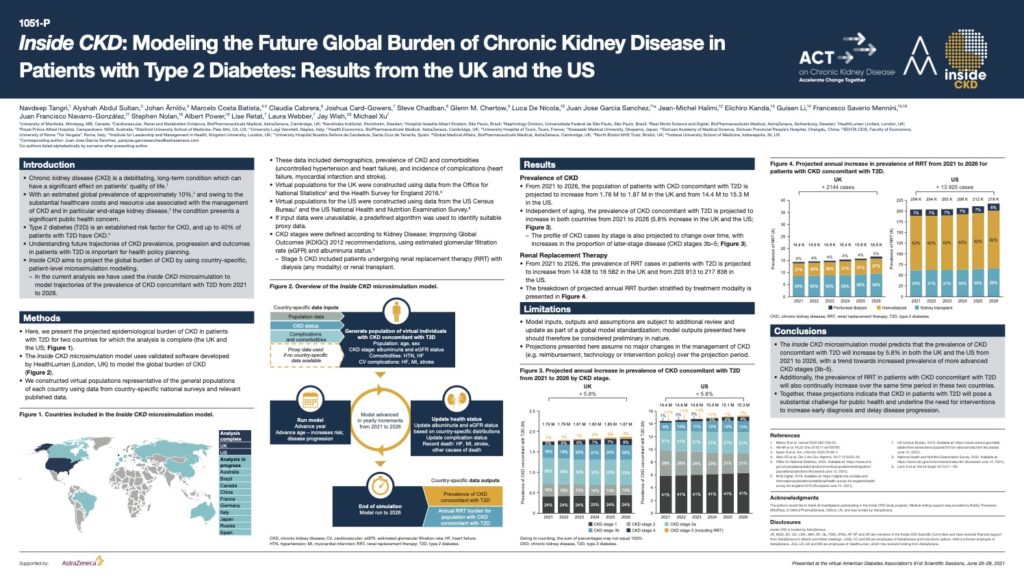
Inside CKD: Modelling the Future Global Burden of Chronic Kidney Disease in Patients with Type 2 Diabetes
Type 2 diabetes (T2D) is an established risk factor for CKD, and up to 40% of patients with T2D have CKD.
This poster, presented at the virtual American Diabetes Association’s 81st Scientific Sessions, June 25–29, 2021 demonstrates that from 2021 to 2026, the population of patients with CKD concomitant with T2D is projected to increase from 1.76 M to 1.87 M in the UK and from 14.4 M to 15.3 M in the US.
These projections indicate that CKD in patients with T2D will pose a substantial challenge to public health and underline the need for interventions to increase early diagnosis and delay disease progression.
Making Conversations Count for All: Benefits of improving delivery of smoking cessation interventions for different socioeconomic groups.
This study builds on the previous 2020 report by looking at the impact of improving the delivery of three advice-based interventions on different socioeconomic groups, compared with current policy, between 2019-2039. By focusing on socioeconomic status, this study explores one component of deprivation to assess the impact of improving the delivery of these interventions on smoking related health inequalities and associated economic costs in the UK.
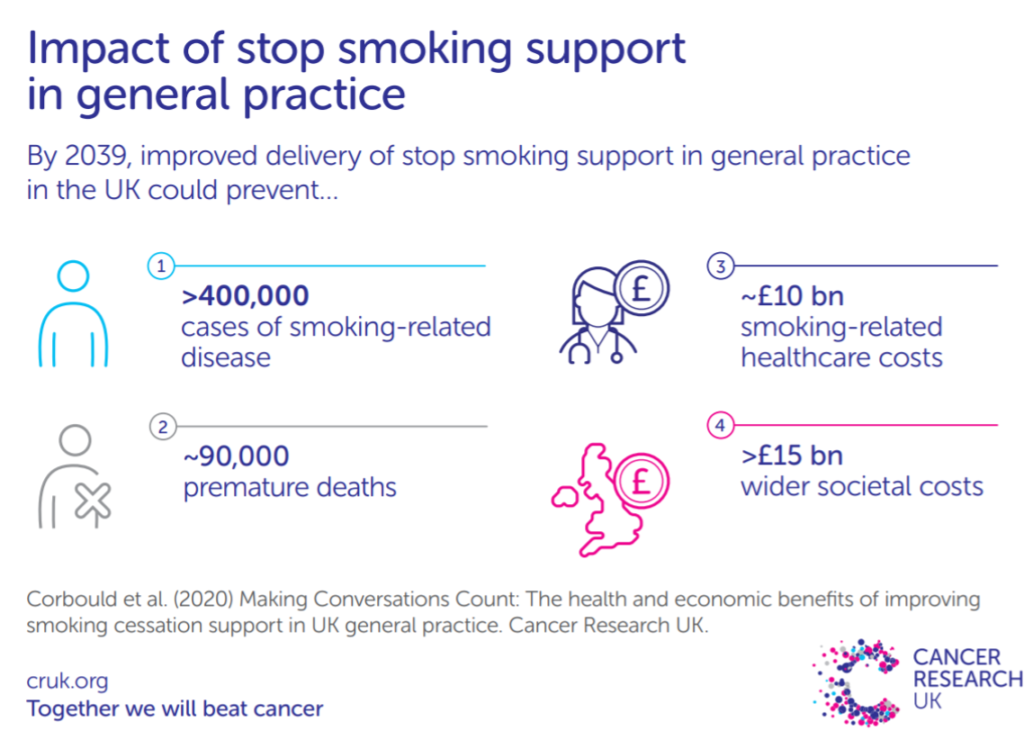
Making Conversations Count: The health and economic benefits of improving smoking cessation support
This study conducted with Cancer Research UK aimed to quantify the health and economic benefits of GPs routinely delivering stop smoking support to patients during consultations in the UK. Using a microsimulation model over the period 2019 to 2039, a current practice 'baseline' scenario was compared to three opt-out smoking cessation intervention scenarios.

Measuring the health impact of Universal Basic Income
In 2019, we reviewed Universal Basic Income (UBI) trial design and findings in comparison with the social gradient in health literature and biopsychosocial theory to identify knowledge gaps. The findings highlight a need to refocus UBI trials on improved health, including via reduced stress, to provide policy makers the means of producing accurate cost-benefit analysis. Previous trials have either not reflected likely UBI policy or failed to measure impacts that enable accurate analysis.
The long-term health impacts of changing exposure to air pollutants in London
Transport for London (TfL) and the Greater London Authority (GLA) commissioned HealthLumen to quantify the health impacts of policies designed to reduce levels of air pollution and improve long-term health. This 2020 study estimates the number of new cases of disease and the resulting costs to the NHS and social care system under three scenarios from 2016 to 2050. The results from this study show that the ULEZ policies and broader, more all-encompassing LES policies have important impacts on the health of Londoners.
REBALANCE: Mixed-methods systematic review and economic evaluation for severe obesity
A study to systematically review bariatric surgery, weight-management programmes (WMPs) and orlistat pharmacotherapy for adults with severe obesity, and evaluate the feasibility, acceptability, clinical effectiveness and cost-effectiveness of treatment.

Obesity in primary care: Screening and brief intervention
The Brief Intervention for Weight Loss Trial enrolled consecutively attending primary care patients who were obese and participants were randomised to physicians opportunistically endorsing, offering, and facilitating a referral to a weight loss programme (support) or recommending weight loss (advice). We use a cohort simulation to predict effects on disease incidence, quality of life, and healthcare costs over 20 years.