It is estimated that a staggering 1 in 10 people worldwide are living with kidney disease (1). Despite its high global prevalence and mortality, CKD has surprisingly often been overlooked on health agendas across the globe up until now.
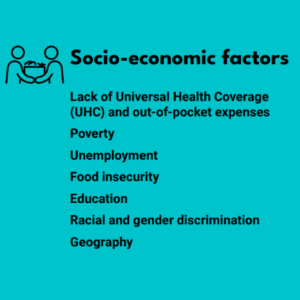
In particular, low and middle-income countries are disproportionately affected by CKD and kidney failure, with a multitude of determinants leading to this disparity in kidney disease burden – including socioeconomic, environmental, cultural and political factors. To bring awareness to this issue, the campaign theme for World Kidney Day this year is focusing on ‘Advancing equitable access to care and optimal medication practice’ to shine a light on the barriers that many face in accessing kidney care worldwide, and to advocate for change.
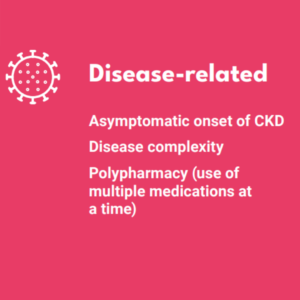
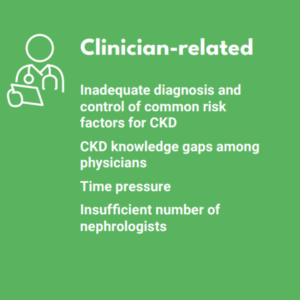
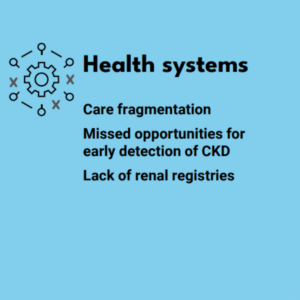
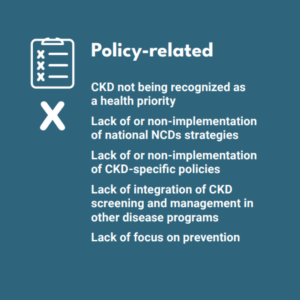
The World Kidney Day campaign has categorised these barriers broadly into six major categories: disease-related, patient-related, clinician-related, socio-economic factors, health systems, and policy-related factors.
Importantly, a number of these barriers can result in delayed kidney disease diagnosis, whether this is due to the typically asymptomatic nature of early-stage CKD, lack of clinical guidelines concerning CKD, lack of access to care in remote regions, or beyond. This represents a significant issue, as CKD quickly becomes harder to treat as it progresses, and increasingly more costly (2), with dialysis and kidney transplants required at end stage kidney disease.
Further, a large proportion of CKD cases could be prevented by addressing social and structural determinants of health, promoting healthy lifestyles, prevention and control of risk factors, avoidance of acute kidney injury, optimization of maternal and child health, and mitigation of climate change (3). This should provide international motivation to bring forward comprehensive public health measures, implement earlier detection and treatment of CKD, and provide affordable access to earlier care.
The need for this is urgent, as demonstrated in HealthLumen’s partnership with AstraZeneca on the Inside CKD workstream within the wider Accelerate Change Together (ACT) on CKD programme, where microsimulation modelling was used to predict the future health and economic burden of CKD from 2021 to 2026 across 31 countries (2). Our work indicated that, if current trends stay constant, CKD is predicted to pose a significant and increasing problem across all countries studied. In the US, for example, a 27% increase was predicted in the number of people with moderate to severe CKD from 2021 to 2026 (4).
When exploring the potential of setting up screening programmes to diagnose CKD in its earliest stages, it was found that such interventions have enormous potential to reduce the burden of CKD across all countries in the study. Taking the US again as an example, when modelling across the 2020 to 2025 period, it was found that routine urinary albumin-to-creatinine ratio screening during primary care visits, followed by appropriate intervention, could prevent progression to CKD stages 3b-5 in approximately 1.3 million patients (5).
Not only is early diagnosis to prevent or delay disease progression in CKD important for patients and their caregivers, but it also could mean alleviating the significant global economic burden that CKD currently poses. Without any interventions, the Inside CKD study found that the total cost of managing all aspects of CKD was projected to increase by 11.6% to $168.3 billion in the US from 2021 to 2026 (4). Half of these costs were associated with end-stage renal disease, highlighting again how important it is to slow progression to advanced disease.
Another major concern regarding CKD is that multiple comorbidities and complications can accumulate over time in patients (6), with concomitant type 2 diabetes being a major risk factor for CKD, and CKD being a major risk factor for cardiovascular disease, for example.
In the US, the prevalence of comorbid gout and CKD is high, which also poses a large health burden on patients and healthcare systems (7). In a recent microsimulation study, we aimed to project the future clinical and economic impacts from 2023 to 2035 of a potential serum urate lowering treatment to control gout in CKD patients in the US. The modelling found that, under a treatment intervention scenario, 353,000 more gout cases were controlled and $27.8B was saved cumulatively through to 2035, compared to the baseline scenario (8).
Ultimately, what studies such as these consistently show is that the time to act is now. There is powerful evidence that strategies in managing the future global burden of kidney disease hold vast potential by focusing on implementing early detection methods, optimizing therapeutic management of kidney disease, ensuring access to medicines, and elevating the quality of care that kidney disease patients receive.
References:
- A single number for advocacy and communication—worldwide more than 850 million individuals have kidney diseases
- Global Economic Burden Associated with Chronic Kidney Disease: A Pragmatic Review of Medical Costs for the Inside CKD Research Programme
- The global burden of kidney disease and the sustainable development goals
- Inside CKD: projecting the economic burden of chronic kidney disease using patient-level microsimulation modelling
- Inside CKD: modelling the impact of improved screening for chronic kidney disease in the Americas and Asia-pacific region
- Reducing the costs of chronic kidney disease while delivering quality health care: a call to action
- Reduced Glomerular Function and Prevalence of Gout: NHANES 2009–10
- Present and Future Health and Economic Burden of Controlled and Uncontrolled Gout in Patients with Chronic Kidney Disease in the United States