In partnership with AstraZeneca, HealthLumen has recently published two publications that project the clinical (1) and economic (2) burden of Chronic Kidney Disease (CKD) and Kidney Replacement Therapy (KRT) into the future, as part of the “Inside CKD” programme, which contributes to the major strategic initiative at AstraZeneca dedicated to driving better patient outcomes.
From 2022 to 2027, CKD prevalence is projected to increase by 5.8% across the 31 regions/countries studied (expanding across the Americas, Europe, Middle East and Asia–Pacific regions) (Figure 1), rising to 436.6 million cases by 2027. Furthermore, the number of patients on kidney replacement therapy (KRT) is projected to increase by 7.7% from 2022 to 2027.
Figure 1: Countries included in the Inside CKD study
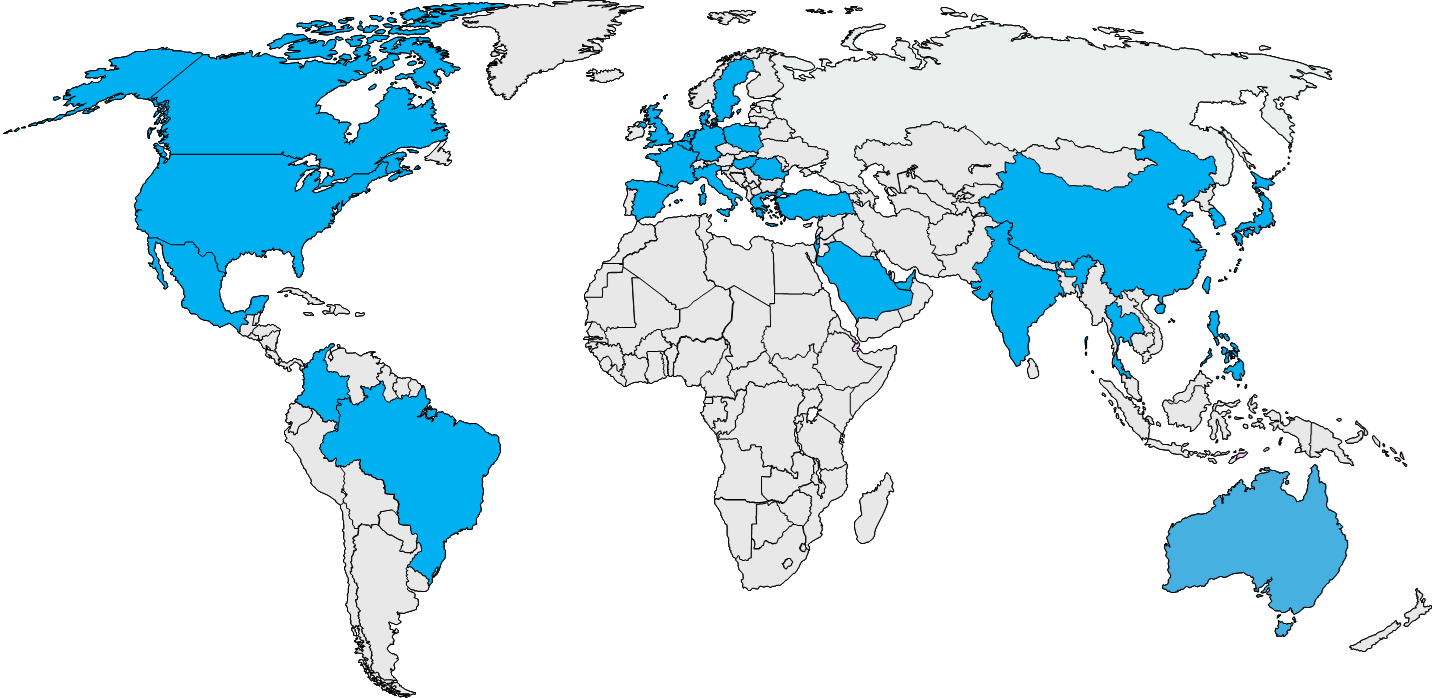
Countries included: Australia, Belgium, Brazil, Canada, China, Colombia, Denmark, France, Germany, Greece, Hungary, India, Israel, Italy, Japan, Mexico, Netherlands, Philippines, Poland, Romania, Saudi Arabia, Singapore, South Korea, Spain, Sweden, Taiwan, Thailand, Türkiye, UAE, UK, USA
Projected economic impacts show that annual direct costs of diagnosed CKD and KRT would increase by 9.3% between 2022 and 2027, from $372.0 billion to $406.7 billion, across the 31 countries/regions. The US bears the largest burden, with costs increasing from $161.9 billion in 2022 to $173.4 billion in 2027. By 2027, CKD and KRT direct costs are expected to constitute 6·4% of healthcare expenditure across the study regions, up from an average of 5·6% in 2022 (Table 1).
Table 1: Healthcare spend for diagnosed CKD and KRT cost across 31 countries/regions
| Costs | 2022 | 2027 | % change |
| Total direct costs | $372.0 billion | $406.7 billion | +9.3% |
| Direct costs in the US | $161.9 billion | $173.4 billion | +7.1% |
| Direct healthcare costs as a proportion of healthcare expenditure across 31 countries/regions | 5.6% | 6.4% | +14.3% |
Particular attention should be drawn to the finding that, although patients receiving KRT are expected to constitute just 5.3% of the diagnosed CKD population across the 31 study countries/regions in 2027, this represents 45.9% of the total costs – highlighting that early CKD diagnosis and proactive disease management to slow disease progression are imperative not just to improving patient outcomes, but also to curb the high costs associated with late-stage CKD.
Further, the Inside CKD study reports that, of the 436.6 million CKD cases expected by 2027, approximately 80% will remain undiagnosed. As a result, assuming current diagnostic protocols remain unchanged, most of the CKD population in 2027 will not be treated. This is a major cause for concern and a key driver for earlier diagnosis, since all-cause mortality rate in the undiagnosed CKD population is over double that of the diagnosed population. Significant numbers of cardiovascular complications among CKD patients were also projected, with an average incidence of 8,859 cases of heart failure, 10,244 cases of myocardial infarction, and 7,797 cases of stroke cases per 100,000 CKD patients across the 31 regions and countries by 2027.
How was this study carried out?
Inside CKD used HealthLumen’s peer-reviewed and extensively validated microsimulation-based computer model to project the future clinical and economic burden of CKD and KRT.
Microsimulation is a form of modelling based on computer-generated “virtual populations” that reproduce the characteristics and behaviour of a large sample of individuals representing the whole population of interest. Particular strengths of the microsimulation-based approach are the granularity, modelling at the level of the individual, and the dynamic nature i.e. the ability to take into account any changes in the characteristics or behaviours of individuals over their life course to model the future burden of disease under different scenarios.
CKD is a debilitating, long-term condition that affects 10–15% of the global adult population (3), and that becomes harder and more expensive to treat as it progresses, with end-stage kidney disease requiring dialysis and kidney transplantation. CKD is also considered a “disease multiplier”: once diagnosed, it is associated with adverse cardiovascular events, including stroke (4), myocardial infarction (5), and heart failure (6). CKD is associated with lower health-related quality of life and higher risk of premature death, which are further negatively impacted by comorbidities, health complications and major health events (7,8).
Due to these factors, CKD poses significant health and economic challenges worldwide, and the key results of the Inside CKD studies provide a clear indication, and warning, that, without intervention, a significant global increase in CKD prevalence, clinical burden, and related costs are projected from 2022 to 2027. This data serves as a crucial tool for shaping future policy interventions aimed at tackling the prevalence, and clinical and economic impacts of CKD across the globe.
References:
- Projecting the clinical burden of chronic kidney disease at the patient level (Inside CKD): a microsimulation modelling study
- Projecting the economic burden of chronic kidney disease at the patient level (Inside CKD): a microsimulation modelling study
- Global, regional, and national burden of chronic kidney disease
- Low glomerular filtration rate and risk of stroke: meta-analysis
- Chronic kidney disease and risk of incident myocardial infarction and all-cause and cardiovascular disease mortality in middle-aged men and women from the general population
- Heart Failure Increases the Risk of Adverse Renal Outcomes in Patients With Normal Kidney Function
- Health related quality of life utility weights for economic evaluation through different stages of chronic kidney disease: a systematic literature review
- Impaired kidney function is associated with lower quality of life among community-dwelling older adults